|
|
||||||||||||||||||
Maintaining a consistent big picture: Meaningful Use of a Web-based POC EHR System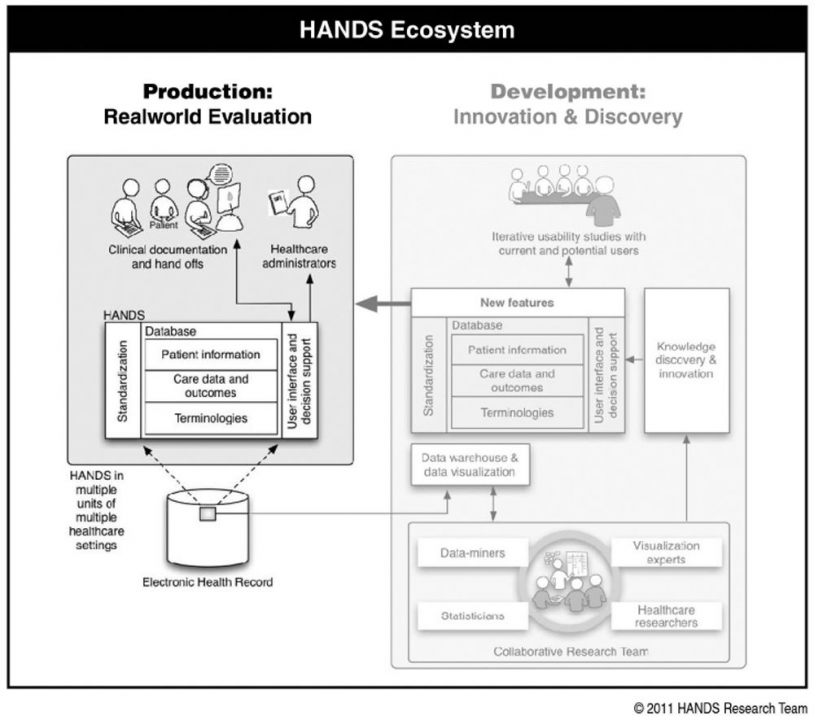
Authors: Keenan, G., Yakel, E., Yao, Y., Xu, D., Szalacha, L., Tschannen, D., Ford, Y., Chen, Y., Johnson, A., Dunn Lopez, K., Wilkie, D.
Publication: International Journal of Nursing Knowledge, vol 23, no 3, pp. 119-133 URL: https://doi.org/10.1111/j.2047-3095.2012.01215.x Objective: To test the hypothesis that Hands-on Automated Nursing Data System (HANDS) “big picture summary” can be implemented uniformly across diverse settings, and result in positive registered nurse (RN) and plan of care (POC) data outcomes across time. Design: In a longitudinal, multisite, full test study, a representative convenience sample of eight medical-surgical units from four hospitals (one university, two large community, and one small community) in one Midwestern state implemented the HANDS intervention for 24 (four units) or 12 (four units) months. Measurements: (a) RN outcomes-percentage completing training, satisfaction with standardized terminologies, perception of HANDS usefulness, POC submission compliance rate. (b) POC data outcomes-validity (rate of optional changes/episode); reliability of terms and ratings; and volume of standardized data generated. Results: One hundred percent of the RNs who worked on the eight study units successfully completed the required standardized training; all units selected participated for the entire 12- or 24-month designated period; compliance rates for POC entry at every patient hand-off were 78-92%; reliability coefficients for use of the standardized terms and ratings were moderately strong; the pattern of optional POC changes per episode declined but remained reasonable across time; and the nurses generated a database of 40,747 episodes of care. Limitations: Only RNs and medical-surgical units participated. Conclusion: It is possible to effectively standardize the capture and visualization of useful “big picture” healthcare information across diverse settings. Findings offer a viable alternative to the current practice of introducing new health information layers that ultimately increase the complexity and inconsistency of information for frontline users. Date: October 1, 2012 Document: View PDF |