|
|
||||||||||||||||||
Spatially-aware clustering improves AJCC-8 risk stratification performance in oropharyngeal carcinomas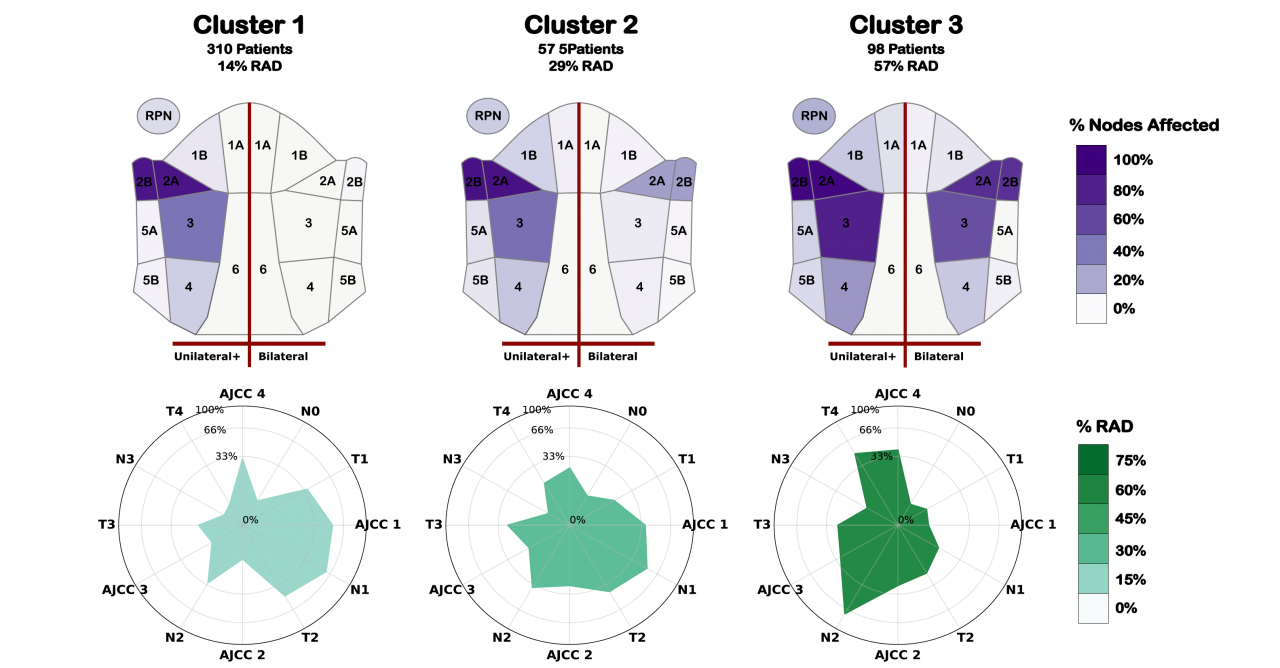
Authors: Canahuate, G., Wentzel, A, Mohamed, A.S.R., van Dijk, L.V., Vock, D.M., Elgohari, B., Elhalawani, H., Fuller, C.D, Marai, G.E.
Publication: Oral Oncology, vol 144, www.elsevier.com/locate/oraloncology, Elsevier Ltd. URL: https://doi.org/10.1016/j.oraloncology.2023.106460 Objective: Evaluate the effectiveness of machine learning tools that incorporate spatial information such as disease location and lymph node metastatic patterns-of-spread, for prediction of survival and toxicity in HPV+ oropharyngeal cancer (OPC). Materials & methods: 675 HPV+ OPC patients that were treated at MD Anderson Cancer Center between 2005 and 2013 with curative intent IMRT were retrospectively collected under IRB approval. Risk stratifications incorporating patient radiometric data and lymph node metastasis patterns via an anatomically-adjacent representation with hierarchical clustering were identified. These clusterings were combined into a 3-level patient stratification and included along with other known clinical features in a Cox model for predicting survival outcomes, and logistic regression for toxicity, using independent subsets for training and validation. Results: Four groups were identified and combined into a 3-level stratification. The inclusion of patient stratification in predictive models for 5-yr Overall survival (OS), 5-year recurrence free survival, (RFS) and Radiation associated dysphagia (RAD) consistently improved model performance measured using the area under the curve (AUC). Test set AUC improvements over models with clinical covariates, was 9 % for predicting OS, and 18 % for predicting RFS, and 7 % for predicting RAD. For models with both clinical and AJCC covariates, AUC improvement was 7 %, 9 %, and 2 % for OS, RFS, and RAD, respectively. Conclusion: Including data-driven patient stratifications considerably improve prognosis for survival and toxicity outcomes over the performance achieved by clinical staging and clinical covariates alone. These stratification generalize well to across cohorts, and sufficient information for reproducing these clusters is included. Keywords: Head & Neck cancer, Statistical and research methods, Machine learning, Radiation oncology, Health Informatics, Imaging, Risk stratification, Oropharyngeal cancer, Clustering, Radiomics Date: June 28, 2023 Document: View PDF |